Abstract
Introduction: Aside of their hemostatic role, platelets have pleiotropic effects and play a role in acute conditions, including host defense against various pathogens. Therefore, the initial platelet count upon acute hospital admission might be a prognostic marker for mortality. This prediction study assessed the relation between platelet count upon acute admission to internal medicine units and mortality.
Methods: We included all adults (>15 years old) in the North and Central Denmark Regions who had a first-time acute admission to an internal medicine unit during 2006-2012. We categorized the patients according to their platelet count measurements within +/- 24 hours of admission, as follows: severe (<50 x 109/L), moderate (50-99 x 109/L), and mild thrombocytopenia (100-149 x 109/L); and mild (401-499 x 109/L) and severe (≥500 x 109/L) thrombocytosis. Within the normal range (150-400 x 109/L), we categorized platelet counts by 50 x 109/L groups. We assessed the association between platelet count and in-hospital, 30-day, 90-day, and 365-day mortality using age- and sex-adjusted Cox models including categories of platelet counts and also using spline regression. We stratified additional analyses by presence of comorbidity (yes/no), defined as any condition in the Charlson Comorbidity Index. We also restricted an analysis to patients with a primary discharge diagnosis of cardiovascular disease vs. infection. In sensitivity analyses, we adjusted for hemoglobin level and leukocyte count upon admission.
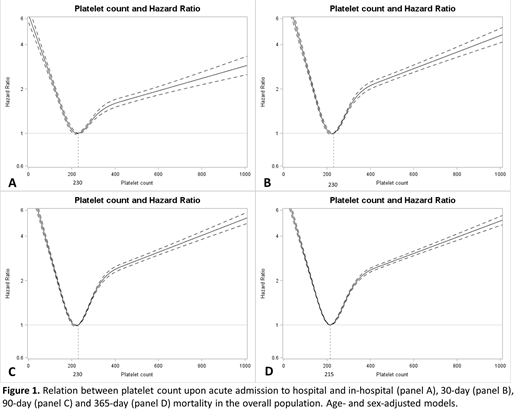
Results: Among the 274,148 patients, 6.8% had thrombocytopenia and 7.8% had thrombocytosis. The association between platelet count and mortality took the form of an asymmetric U-shaped curve, more marked for thrombocytopenia (Figure). For 30-day mortality, the hazard ratios (HRs) were 5.24 (95%CI 4.60-5.97), 3.77 (95%CI 3.43-4.14), and 1.63 (95%CI 1.52-1.74) for severe, moderate, and mild thrombocytopenia, respectively; and 1.91 (95%CI 1.79-2.04) and 2.50 (95%CI 2.33-2.69) for mild and severe thrombocytosis (reference group: normal platelet range). Compared with patients in the 200-249 x 109/L category, mortality was at least slightly higher in patients with a platelet count between 150-199 x 109/L (HR 1.13, 95%CI 1.06-1.21), between 250-299 x 109/L (HR 1.12, 95%CI 1.05-1.19), between 300-349 x 109/L (HR 1.38, 95%CI 1.29-1.47), and between 350-400 x 109/L (HR 1.82, 95%CI 1.69-1.96). A similar pattern was observed for in-hospital, 90-day, and 365-day mortality, among patients with and without comorbidity, and among those with a primary discharge diagnosis code of cardiovascular disease. Among patients with a primary discharge diagnosis code of infection, a platelet count between 150-199 x 109/L was associated with decreased mortality. Sensitivity analyses adjusted for hemoglobin level and leukocyte count upon admission yielded similar results.
Conclusions: Both thrombocytopenia and thrombocytosis are markers of increased mortality up to one year after hospitalization in an internal medicine unit. Even within the normal range, low and high platelet counts were associated with slightly increased mortality. The lower mortality in patients with infectious diseases who had a platelet count between 150-199 x 109/L may reflect appropriate platelet consumption in host defense against pathogens.
Christiansen:Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal